A 55 yr old male with complaints of abdominal pain and shortness of breath
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome
A 55 yr old male patient who is resident of kammagudem came to the casuality with
Chief complaints :
Abdominal pain since 5 days
Breathing difficulty since 2 days
History of present illness:
Patient was apparently asymptomatic 5 days back then he developed abdominal pain after taking alcohol continuously for 3 days . It is sudden in onset and gradually progressive and dragging type which is aggravated on alcohol intake and relieved on medication. Previously visited other hospitals before after onset of abdominal pain but it didn't relieve inspite of medication .
There is h/o altered sensorium since 3 days . He is unable to identify his wife and pulling away the cannulas.
There is history of nausea where he vomited by inducing with his hand .
There is history of weight loss also since 1 year.
History of sob which is grade 4
History of fever yesterday.
Past history:
A known case of diabetes since 2 years on medication .
History of TB diagnosed 2 months back on regular medication.
Not a known case hypertension,asthma,epilepsy,CVD.
Personal history:
Bowel and bladder - regular and there is increased frequency of urine seen when sugar levels are increased .
Not sleeping adequately since 2 days
Alcohol consumption since 30 yrs occasionally for festivals but he drinks continuously for 3 days of 1 full bottle quantity.
History of tobacco smoking since 25 yrs.
Family history:
Not significant
Examination of elderly male patient .
General examination:
Patient is conscious ,not co operative ,not oriented to time place person
Not well built and nourished .
Afebrile
GCS :
EYE OPENING :4 (opened spontaneously)
VERBAL RESPONSE: 3
MOTOR RESPONSE :3
Total :10
Pallor : present
Icterus : absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy : absent
Vitals:
Pulse - 90bpm
RR - 22 cpm
Bp- 140 / 70 mm hg
Temperature- 97.4°c
Systemic examination:
Examination of oral cavity-
No dental caries, no gum hypertrophy , oral hygiene is maintained , no postnasal drip
Abdominal examination-
INSPECTION:
Shape – scaphoid, flat,not distended
Flanks – free
Umbilicus – Position- central, Shape-inverted
Skin – No scars, no sinuses,no striae, no nodules,no scratch marks,
Dilated veins – not present
All quadrants are equally Movable with respiration ,no visible gastric peristalsis.
No abdominal distension .
PALPATION:
No local raise of temperature.
Superficial Palpation – Tenderness not elicited.
Deep Palpation-
Liver-
Not palpable
Spleen-
Not palpable
Kidney-
Bimanually Not palpable
PERCUSSION:
Fluid Thrill/Shifting dullness/Puddle’s sign - not elicited
Liver span - 6cm
AUSCULTATION:
Bowel sounds are heard.
EXAMINATION OF OTHER SYSTEMS
CARDIOVASCULAR SYSTEM:
S1, S2 are heard.
EXAMINATION OF RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
EXAMINATION OF NERVOUS SYSTEM:
Altered sensorium, irrelevant talking and unable to recognise his wife and He is pulling away the cannula.
GRBS : (On 8 th jan ) inj HAI 6IU IV/STAT followed by insulin infusion.
5:30-600 mg/dl
7:30- 390 mg/dl
8:30-380 mg/ dl
9:30- 383 mg/ dl
10:30- 382 mg/dl
11:30- 260 mg/ dl
12:30- 210 mg/dl
1:30- 220mg/dl
2:30- 206 mg/ dl
3:30- 207 mg/dl
4:30- 147 mg/dl
5:30- 77 mg/dl
6:30- 121 mg/dl
7:30- 131 mg/dl
On 9 th jan :
On 11 Jan :
Patient reviewed
Pain decreased yesterday denies for alcohol cravings.
On examination- patient drowsy
Bp - 110/70 mmHg
PR-102 / min
SpO2 - 98% on room air
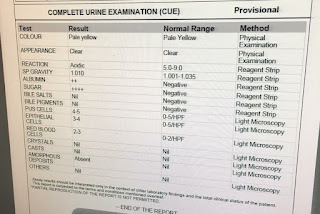
Lab investigations-
ABG analysis:
pH -7.44
PCo2 - 25.3
HCO3 - 17.1
Serum urea - 47
Serum creatinine- 0.8
Na+ - 133
K+ - 3.2
Cl- - 94
1. IVF- NS- 1L for 3hrs.
2. Inj HAI 6IU IV/STAT followed by insulin infusion.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.
PROVISIONAL DIAGNOSIS:-
Diabetic ketoacidosis with known case of diabetes milletus.











Comments
Post a Comment